- One must wait until the sunset to see how splendid the day has been.
- Anon.
The surgeon did not pussyfoot around about the likelihood of my dying. He said that half the people with my disease were alive one year after diagnosis. Only three out of a hundred were alive five years later. The night I found out the diagnosis, I scribbled down a list of dreaded tasks that I would never have to do again—
- give large dinner parties
- clean the oven
- scrub floors
- wash delicate things by hand
- remove stains.
The second thing that I did was to get a calendar and try to figure out a convenient time for me to die.
Then I made a list of people who are already dead, people I would enjoy seeing. I drew it up like a list for a cocktail party.
Until my surgeon told me that I was dying, I never cared much for euphemisms. I preferred the word “dying,” for instance, to “passing on” or “going to sleep in the Lord.” Now, however, I’ve decided that dying is a word that absolutely requires a euphemism if you’re about to do it.
People recoil if I tell them that I’m about to die. They (and I) feel better if I say I’m about to “kick the bucket” or to “check out” or to “bow out.” It’s not the metaphorical humor of these euphemisms that makes them more acceptable socially. It’s rather, I think, that they describe a familiar scene. All of us at some time have kicked a bucket or checked out or bowed out. But none of us has ever died. Moreover, kicking the bucket and checking out and bowing out are positive actions that we have taken cheerfully and vigorously at a time that suited us.
Things to be glad about while dying of cancer:
- I don’t have to worry about getting cancer anymore. (I always expected to get cancer of the foot because of the X-ray machines that we played with in shoe stores when I was a little girl.)
- I had a wonderful trip to Jamaica.
- I don’t have to worry about gray hair. I don’t have to worry about rosacea.
There are only two REAL benefits.
- I found out that people love me who I would never have guessed love me. I would have died without knowing.
- I won’t have to learn the metric system.
Having cancer is, as it happened in my case, a pain in the lung—a particularly unjust location for my cancer since I have never smoked a cigarette in my life. My parents, also nonsmokers, reared me in Winston-Salem, North Carolina, the tobacco capital of the world. Like many people in Winston-Salem, my parents owned some stock in Reynolds Tobacco Company.
When my lung malignancy was first diagnosed, I began to wonder why I had been afflicted with this particular malignancy by Whoever’s In Charge of Distributing Cancer, hereinafter referred to as WICODCA. I’ve never believed that the Lord is in charge of that sort of thing. I decided that WICODCA, having failed to ruin the cigarette industry by giving smokers cancer of the lung, decided to afflict the children of stockholders. I had visions of a surgeon-general’s warning, printed on the bottom of tobacco company stock certificates: “The Surgeon General of the United States has determined that owning stock in cigarette companies is a danger to the health of your children.”
WICODCA is housed in an inconspicuous brick building near McLean, Virginia, jointly financed by a grant from HEW, NIH, and ACS. No one works there except technicians who keep the computers working properly and secretaries who mail out computer print-out sheets when they are requested. No one knows who feeds the information into the computer—it appears in the night. On the night of Oct. 11, 1978, my name was fed into the computer:
(The cause is often speculated upon, with other patients; for examples, “heavy smoker for 18 years” or “worked with asbestos” or “mother took DES while carrying this child,” etc. )Molly Ingle Michie 243—54—7152
October 4, 1932, female, multipara,
Caucasian, housewife,
Charlottesville, Virginia
Broncho-alveolar cell carcinoma
CAUSE UNKNOWN
HEW, NIH, and ACS obviously are not pleased with having the source of the information a mystery. They have at various times considered canceling funding of the operation because of this peculiarity. But the information is extremely valuable, up-to-date, and accurate. Assembling the data from hospitals around the country would be more time-consuming and expensive. They have conducted studies for accuracy. When information coming directly from WICODCA is compared to information coming from hospitals, it has been found that the hospital information contains many errors. Also the follow-up on WICODCA is immediate and accurate. In the night, death notices and five-year “cures” are fed in. Responses of various patients to various treatments are also available.
A circle of love formed itself around my bed there in the hospital. No one withdrew or said the wrong thing. Their sorrow was obvious; their strength was apparent and available without my asking. Nothing that I would need—emotionally, physically—would be denied to me.
The hospital staff was uncannily tactful. They cared that I hurt, and they were eager to help. A chaplain came in the next morning. She had done her homework. She knew I was a Unitarian and that she couldn’t assume that I would welcome her. She did a beautiful job. She asked open-ended questions that really required no responses from me—just sort of puzzlements about tragedies and sorrows. She let me know subtly that she thought there were some comforting answers and that she would share those answers any time I called. Then she left—a perfect job, under very difficult circumstances.
I had read Elisabeth Kubler-Ross’s classic Death and Dying during the summer—certainly not in anticipation of my own death but because so many of my relatives are 70 and 80 and obviously concerned with the prospect of dying. As I read the book, however, I did think of myself and what my reactions would be if I learned I had a terminal illness. Kubler-Ross describes five phases: denial, anger, bargaining, depression, acceptance. I decided that I would probably skip the first three phases and plunge headlong into a deep depression. The denial and anger and bargaining stages seemed too irrational for a cool-headed lady like me. Facts are facts, malignant cells are malignant. “Why me?” is so obviously answered by “Why not me?” Getting mad at God seemed so childish.
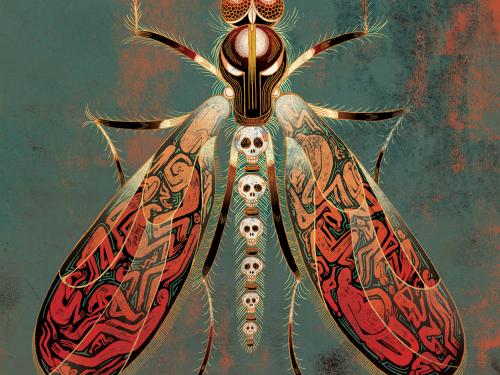
But anger came in a strange free floating form. There must be someone to blame, someone who robbed me of precious time—the very prime of my life. My anger, free floating, gradually took an animal form. A tiny albino falcon appeared over the door of my hospital room, a vicious fellow with pink eyes and long pink talons. I named him A. F. , which stood for Albino Falcon and for Anger, Free Floating. He was ready to attack anyone who abused me in any way-—callous nurses, bearers of inedible meals, inconsiderate visitors, or cleaning personnel who might wake me from a nap.
He rode on the back of my wheelchair or stretcher when I was transported for tests or examinations, looking for callousness or carelessness in any form. For four days no one was callous or careless. A. F. was getting frantic and larger. He began flapping wildly around the room. Clearly he would have to attack an innocent, if a proper villain could not be found soon.
Monday morning the nurse announced that at 1:30 that afternoon I had an appointment at radiation oncology where I would discuss a proposed course of radiation therapy. A. F. and I were jubilant—a perfect villain! A. F. and I settled down, he to sharpen his talons and I to ponder my hatred of radiation and all doctors and technicians who practiced it.
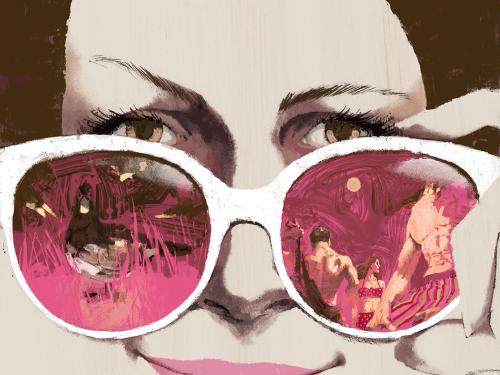
When I graduated from Hollins College in June 1954,1 was given by my parents a glorious graduation present, summer school at Oxford University. Tom happened to attend that summer session also. We rode up from London on the same train, met briefly in the station, and caught the same ride to our dorm at St. Hilda’s College. By the time the session was over, we were fairly sure that we were in love. We decided, however, not to make any long-term commitments until we had seen each other on home turf. The romantic spires of Oxford might have made anybody seem a delightful prospective spouse. But Tom looked even better to me surrounded by friends on the grounds of the University of Virginia, and by his attractive relatives at his father’s home in Charlottesville, than he had punting down the Cherwell at Oxford. Tom liked my parents and friends in Winston-Salem, too. We decided definitely to marry.
He was starting his second year at the University of Virginia law school, and I was looking forward to my first job as an assistant librarian at Bowman Gray Medical School in Winston-Salem. One of my duties was to gather articles and books for doctors who were preparing papers for medical journals. Dr. Richard L. Masland, professor of neurology, asked me one day for a stack of articles on the possible causes of Down’s syndrome. Because of my impending marriage and my enthusiasm for many healthy babies, I was fascinated in a horrible sort of way by the articles I gathered.
Some of them speculated that the cause was a particular disaster that occurred to the mother during the eighth week of pregnancy—perhaps an operation involving anesthesia or a sudden blood loss or the mother’s being somehow deprived of oxygen by smoke inhalation or strangling on a piece of food. One article said that medical X-rays to the abdomen of pregnant women might be the cause of several birth defects— blood disorders and Down’s syndrome among them. During slow times in the library, I actually started looking up articles about the detrimental effects of radiation and deciding that neither I nor Tom nor any of our children would ever be Xrayed. I developed a full-blown, somewhat irrational phobia about X-rays.
The Navy hospital where I received prenatal care for our first child, Tommy, required a chest X-ray of each mother. I had mine taken with tears running down my cheeks. After the children were born, the perversity of nature and the Fates manifested itself. I was the only mother on the block with an enormous X-ray phobia, yet I was the only mother on the block whose children constantly needed X-rays.
Our first three boys were born in 1957, 1958, and 1959 (on our fourth anniversary we had three children). I had a hard time coping with them all. They were constantly closing each other’s fingers in doors and tripping over toys and having possible concussions. Our second son, John, was born with one foot slightly out of position. Our third son, Ned, had unusual torsion in his thighs (a result of sleeping only on his stomach, as it turned out, but an indication to his pediatrician that there might be a congential hip dislocation). At two, Ned had a positive T. B. test that required many chest X-rays through the years.
George, our fourth son, born in 1964, had a number of accidents requiring X-rays. When he hurt his elbow in gym class, the technician X-rayed his right elbow from three different angles. The doctors still couldn’t tell if there was a break or a peculiarity in his bone structure, so he asked for an X-ray of the left elbow in order to compare. I was constantly being presented with a terrible choice—an X-ray or a deformed elbow. I always had to choose the X-ray. My hatred of X-ray machines and personnel grew. The personnel found me terribly amusing or terribly annoying. I became increasingly paranoid. Would the hostile technician leave the machine on just a little longer than necessary to get even with a troublesome parent?
I discovered a way to avoid a few routine X-rays. John, like Tommy, was born while Tom was in the Navy, and the hospital again required a chest X-ray of me. I noticed that the doctors wrote “negative” by “chest X-ray” on my chart. Then he wrote out an order form and handed it to me. I just tore up the form. So, we always did that on job applications and college health forms, too. Most camps and colleges require only T. B. skin tests now, anyway, but Vanderbilt’s form required an x-ray. On May 9,1975, Tommy’s doctor examined him and wrote May 9, 1975 as date of most recent negative chest X-ray. He handed Tom the X-ray order form, and Tommy left.
Rip!
James Thurber’s grandmother always thought that electricity was leaking out of outlets, and I had that same feeling about radiation seeping out of open X-ray room doors. I always hurried past radiation room doors—holding my breath and hugging the far wall of the corridor. Now I was being wheeled into the radiation room itself. A. F. and I were in a state of wild tension.
Unfortunately, the first person we met was NOT a possible target. She was one of the most beautiful women I’ve ever seen—a Dutch woman, a person of such warmth and sympathy that A. F. immediately flapped off in disgust. Her job, she said, was to make things go smoothly for the patient. She was available for questions or to make contact with the radio-therapist, to adjust medications, to hear complaints—anything I needed I should feel free to ask her. She pushed me into an examining room, chatting, smiling, discovering mutual friends. When I was draped and ready to see the doctor, she left. A. F. returned immediately, perching on a cabinet top.
Into the room came a small, oriental man. A. F. attacked immediately, sinking his pink talons into Dr. Meng L. Lim’s yellow neck. World War II lasted from my ninth to my 13th year. Every Saturday afternoon during that time I went with my friends to war movies. We ate popcorn and watched Japs torture heroic American pilots. I developed a hatred and fear of the Japanese. Here was Dr. Lim—Japanese and a radio-therapist. Already he was talking about how many rads he would need to give me to stop the cancer’s growth. Already his fingers were looking for evidence of new growth. With his yellow, torturer’s mind, I knew he was hoping to find new growth.
I began asking him questions to which I probably did not really want to know the answers. I had refrained from asking them of my surgeon, Ivan Crosby, partly because I didn’t want to know and partly because I like him so much and because he obviously hated to give me bad news. I asked him once during the weekend if my kind of cancer was possibly— hopefully—finicky, liking to eat only pleura exclusively. He shook his head sadly and said, “It’s not very finicky. It likes other things, too.” I did not ask Ivan which other things.
I did ask Dr. Lim immediately. He would enjoy giving me bad news. “If the cancer spreads,” he said, “it will most likely go to your liver or to your brain.” He told me to come back in one week to be marked for radiation treatments on the linear accelerator. An orderly came to wheel me back to my room.
A. F. let go of Dr. Lim’s neck and settled himself on the back of the wheelchair, licking his talons, obviously calmer than before. I felt calmer, too. Some of my anger had found a target. As we were wheeled down the long hall of the radiation oncology department, I began to notice other defects that could absorb some of my anger. The Dutch therapist waved a cheerful goodbye. She was going to make things difficult for A. F. and me, but we would prevail by ignoring her.
Tom’s sister, Emily, is a pretty, vivacious woman seven years younger than he, a talented teacher, mother of three delightful children. She has been married for 20 years to John Gennari. They met while she was at Vassar and he was at Yale and married the year they graduated. She worked in the Yale library while he was in medical school and then began producing a child every two years, while he did his residency and internship here in Charlottesville at U. Va. Medical School. John is handsome, witty, brilliant, and incredibly patient. He’s the only doctor in our immediate family, and we call him for advice, confirmation of diagnoses, comfort. He is a nephrologist, now at the University of Vermont in Burlington, but at the time of my operation he was finishing his tenth year of research at Tuft’s New England Medical Center. John’s willingness to help us enabled us never to seek a second opinion or a fancier medical center. When Dr. Lim prescribed 2000 rads to the full right lung and 2000 to a smaller area where they thought the tumor originated, we called John, who said he would ask the head of his radiotherapy department about the dosage, the machines, and the doctors in that department at the University of Virginia. He called the next night to say that his department head said that she did not know Dr. Lim, but that Dr. William C. Constable, the director of radiation oncology, was internationally known. She said that U. Va. had terrific equipment and that we should do whatever Dr. Constable said.
Tom called Dr. Constable, who agreed to see us that very day. He’s a Scot, with a crisp but kind manner. He seemed slightly bemused by our anxiety but was thoroughly courteous and unhurried. He said that all decisions about dosages are discussed by the entire department, that he personally had gone over my X-rays and treatment recommendations with Dr. Lim, and that the recommendation for dosage and treatment would be the same at any major medical center in the world.
I liked him immediately. He could have been a flight surgeon with the RAF in my war movies. Better still, he had on his bulletin board a copy of Murphy’s Law. I liked being treated by someone who realized that “anything that can go wrong, will.”
I soon found out for myself that the department was impeccably run, that Dr. Lim is not Japanese but Chinese, and that he is a warm, thorough, helpful doctor, with a good sense of humor and a real concern for his patients. A. F. and I, however, retained our hostility toward him while we looked around for other more suitable targets. A. F. always taloned him on sight.
Mark-up on Monday was a nightmare for me. I lay on a hard table, in an incredibly uncomfortable position for someone who had just had a thoracotomy, while pretty, cheerful technicians X-rayed me repeatedly and drew on me with purple magic markers. They would decide that my spine was not exactly straight, move me ever so slightly, and X-ray again. I begged for lead blankets to cover my vulnerable right lung and liver, but they giggled and said there were no lead blankets in radiation oncology. “After all,” said one technician, “you are scheduled for 4000 rads. From these little X-rays you get only a few millirads.” A. F. clawed her lovely cheeks.
Finally I was marked to their satisfaction, told not to remove the purple marks until the ten treatments were over, and released. By this time, all four of the girls had talon scratches on their cheeks. Marked— what a horrible word! How appropriate for such a horrible word to be chosen for use in such a horrible place. A marked man means a doomed man. Why not say I had been decorated with a purple pen— embellished—drawn upon? But marked? Marked is a word in need of a euphemism.
Treatments began the next day. The linear accelerator looks like a machine from Star Wars. I got on its one out-stretched arm, my back resting on an open plastic grid. When I was lying comfortably, the arm would move under the machine itself. Technicians would line up my marks with a pattern on the machine above. Computer lights would flash. The technicians would leave the room. A high pitched sound would begin and last for about 15 seconds. The technicians would return, punch a button, the whole machine would revolve 180 degrees, and I would be zapped through the back for 15 seconds. Then the arm would swing me out again and I would dismount. The technicians were all young and beautiful, cheerful and friendly. They chatted with me and with each other. I was convinced that they chatted and drank coffee while they zapped me, and that whether I was zapped for 15 seconds or 25 depended on the whim of three silly 19-year-olds. A. F. got them all.
The next day Dr. Constable himself came in the treatment room to check the set-up. He waited for me outside. Then he showed me how the machine’s timing was locked into a computer—how warning bells would ring if anything started to go wrong. How a computer printout recorded every rad and every second. Murphy’s Law could not apply to this machine. Nothing could go wrong. A. F. gave him one good scratch for not telling me that the day before.
The next week I met another lovely chaplain. She, like the first one, did not intrude on my privacy in any way. She let me know that she was available for my spiritual comfort and then she talked amicably about many interesting things and said that she was trying to get the patients’ perspective on radiation treatments, so that she could be helpful if they were distressed by some aspect of the procedure. She left me then to talk to another patient.
When later I was in position on the linear accelerator arm, this chaplain appeared. I was somewhat startled, since I was nude to the waist and unaccustomed to being visited by clergy while unattired. When my marks and their pattern were lined up to their satisfaction the technicians left. The chaplain stayed behind a moment, patted me on the arm comfortingly and said, “Remember, we’re with you all the way.” Then she left.
Tears of anger streamed down my cheeks. “You’re not with me,” I wanted to scream. “If you’ve got any sense, you and all those pretty technicians are behind thick lead shields. There’s no one in here being sizzled but me.” A. F. shredded her into bite-sized pieces.
I found one more object to vent my anger on in that department—a squawk box in its reception area. When a patient enters the corridor of the radio oncology department, there is a comfortable-looking waiting room with magazines, pictures, aquariums, etc. on the right. On the left is just a row of chairs lined up against the corridor wall. All of the patients sit in the lined up chairs waiting to hear their names called over the squawk box. The volume is turned very low and there is a lot of static, so no one talks to anyone else for fear of not hearing his name called. If you do miss your name, a friendly lady at a desk nearby will usually say, “Mrs. Michie, I think they called you back.” I never got to know another patient, even though I saw some of them ten or 20 times. We all sat silently, lined up, listening for our names.
Even though I knew that the lovely Dutch therapist was waiting to help, eager to help, I never told her or Dr. Constable or Dr. Lim my complaints. I didn’t tell them because I wanted some targets for my free floating anger. I know from experience that the old poem is true:
“I told my anger to my friend
And telling made my anger end.
I held my anger from my foe
And holding made my anger grow.”
A.F.ripped that squawk box off the wall on our last visit to the beautifully run radiotherapy department. It was a department full of talented, dedicated people who had given me months full of happy hours, months that I could not have expected from any other course of treatment.
Ninety-nine percent of the people in the world, including me, want to die when they’re very old, and, I imagine, a similar percentage would choose to die suddenly. I’ve had to search for satisfactions to be found in dying in middle age—in the prime of life. But satisfactions in dying slowly have been obvious and not hard to find:
I’ve had time, with no demands, to put things in order and to gain perspective.
I’ve never been much of a nature lover, but now that I’m seeing it for the last time I am appreciating it. I’ve had time to watch the woods fill up with snow. I watched spring come twice, first here and then again at Bucknell in Pennsylvania during parents weekend. It was gorgeous.
I’ve had time to savor the good foods of summer—watermelon, cantaloupe, blueberries, peaches, fresh asparagus, corn on the cob.
I’ve had time to view the boys anxiously but calmly, and to see that they are terrific: mature, confident, and capable. My boys talked to me about interesting philosphical questions. I’m sure we would not have talked like that except for my illness. I might have lived to 90 and never have known them so well.
I’ve had time to find out that many people love me— people who I would never have guessed love me.
These satisfactions are not available to some who die slowly. Sometimes the disease is too painful, too disfiguring and distressing, too controlling of body functions to give the victim time for the pleasures I’ve listed. Sometimes the family and friends cannot be supportive because of their own fears and conflicts or because of economic pressures or other circumstances—small children to care for, for example.
I have been fortunate on both counts. I have a relatively painless lung cancer so that my time is not consumed in struggling with discomfort or unpleasant treatments.
My family and friends are incredibly supportive—freeing me from demands and chores, letting me talk and helping me put my thoughts and things in order—an enormous satisfaction—a summing up.
In the nine months between the diagnosis of her disease and her death, Molly Michie was never at a loss for composure, cheer, or courage. And she never went into depression. She died at 2 P. M. on Monday, July 2, 1979, exactly 25 years from the day she first met Tom at the train station in Oxford.