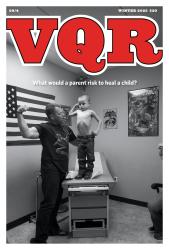
Ten years ago, a woman who had previously received an artificial heart valve at the University of Virginia’s Medical Center saw her local physician in a West Virginia town. Although unknown to anyone at that time, later experience would show this type of valve to be vulnerable to material fatigue and abrupt malfunction. The West Virginia doctor did not like the sound of her valve and called to request an appointment for her the following Monday at the medical center. On Friday night, the weather forecasters predicted a weekend blizzard. Although this physician saw enough patients daily to create a mental blur of pathology at the end of the day, that night he recalled this woman’s plan and telephoned her to suggest that she leave early to avoid the snow. She agreed to do so. As she approached the hospital in a blizzard that Sunday, her valve completely failed. She required emergency valve replacement surgery within the hour to prevent death. The operation was successful, and she returned home well in ten days. What possessed the West Virginia doctor to think in such detail about this patient that he called her at home to suggest a change in her travel plans because of a weather forecast?
A few years ago an elderly professor appeared to be dying of pneumonia in a setting of incurable malignancy and other irreversible problems. Experiencing bone pain in recent months, he had supplemented his codeine with excess vodka for pain relief and had fallen and broken a cancerous bone. Physicians less familiar with his background had inserted a breathing tube, attached him to a respirator, and started antibiotics. My inclination was to remove these supportive measures and allow death to come with compassion and a minimum of discomfort. The problem was gently presented to his wife with a gloomy prediction. She said, however, that her husband had an enormous will to live and would want “everything” done. And so we did everything. Indeed, the man did recover from this episode, and he lived, sometimes even enjoyed, another ten months at home before he succumbed to more of the same.
The events described in the first account are fortunately quite rare, while those in the latter are probably rather common. The first story is not so much a testimony to the wonders of modern cardiac technology, although that did prolong and improve the woman’s life twice, as it is a tribute to the presence of a doctor sufficiently concerned about both the disease and the patient. His consideration of a small detail, like weather and travel, turned out to be a crucial element in a successful outcome. The second story raises many unanswerable questions. Was the ten-month survival for this patient worth it? And worth it for whom? Even allowing that the doctor’s urge to restraint was based on compassion rather than cost considerations, it cannot be ignored that the patient’s extraordinary hospital costs were borne not by him but by fiscally troubled, federally-funded programs.
II
The 20th century has seen a series of reforms or overhauls in the patterns of medical education and practice, each in response to an apparent deficiency and each leading in turn to a new deficiency requiring further reform. At the turn of the century there were relatively large numbers of doctors seeing sick or injured people mostly in homes, offices, and a limited number of hospitals. Later, the emergence of successful surgery, laboratories, and needs for nurses and other assistants would make hospitals become centers of medical organization, communication, and practice.
Most doctors before 1900 had gained scant scientific education from many proprietary, one-year medical schools, and they could offer but little control over the diseases they encountered. The frontier society of the previous century had fostered in the public medical self-reliance, and there was skepticism about the value of medical attention. Acceptance of death and disability was a prevalent means of accommodating reality in the societies of that time.
The first major reform around the turn of the century was in the quality of medical education. Licensure by states was reintroduced, and new physicians were required to know of the many advances in infection control, surgery, diagnostic X-ray, and clinical biochemistry. Medical education became more rigorous and prolonged, which led in turn to smaller numbers of better physicians, while urbanization, improved transportation, and continued scientific and technical progress enhanced the demand for doctors’ services. Thus was set the stage for the next problem—availability and affordability.
As elegantly described in Paul Starr’s The Social Transformation of American Medicine (1982), the educational reforms produced physicians of better scientific quality, but when combined with increased dependence on technology these reforms also enhanced the barriers to medical care for significant sectors of the population. The next reforms were thus directed at increasing public access to medical care, in part by reducing financial barriers. After the 1930’s, growth in medical insurance plans through employers gave protection to many of the working middle class from devastating medical expenses. Such protection was not, however, as readily available to the elderly and poor. Since the early years of the century, the concept of government as guarantor of a reasonable level of citizen welfare has grown throughout the developed world, and many countries have established national health services with state-employed physicians and state-managed hospitals. Resistance in the United States to large-scale organization and regimentation long prevented that step, but by the 1960’s the demands on politics and social compassion required some response on a national scale to the problems of the medically underserved.
Thus in 1965 there appeared in the United States medical entitlement programs—Medicare for the elderly and disabled and Medicaid for the very poor. In an effort to avoid creating a two-class system of medical services, the private, fee-for-service mechanism for paying doctors was retained. Government purchasing of medical care for previously underserved groups mitigated somewhat the problem of access and improved some indices of public health, but the increased demand for physicians’ services was associated with rapidly escalating costs and prices in medical care. As costs have mounted dramatically, restrictions in benefits under government and insurance programs have appeared. The combination of liberal employment benefit programs and government entitlements has become threatened by a combination of high costs, uncertain efficacy, and the loss of consensus into special-interest politics. By 1986, not only had medical expenditures become very high but also 27 percent of the working population were either uninsured or underinsured, and medical care for the poor had returned as a visible and unsolved problem.
III
Most observers agree that a major problem of the 1980’s is the extraordinary expansion in the costs of medical care in the United States. Estimates of U.S. annual health expenditures were $12.7 billion in 1960 (4.5 percent of Gross National Product), $71.6 billion in 1970 (7.3 percent GNP) and $231 billion in 1980 (9 percent GNP). With large proportions of this sum now underwritten by government or by employer-financed insurance plans, a consensus has developed that these costs are intolerable. Medical costs are not so great in other comparable developed countries, which often seem to have as favorable measurements of public health.
Many causes have been advanced for the seemingly uncontrolled medical inflation in America. A partial list of proposed causes suggests the scope of the subject:
- More old people requiring more medical services.
- High development costs for the high-technology gains— artificial human parts and transplants, new diagnostic methods of greater accuracy, more effective drugs, helicopters for emergency transport.
- Physician remuneration patterns favoring performance of expensive procedures.
- Public expectations of uniformly successful restoration of health by means of medical attention.
- A “do-everything-you-can, doctor” philosophy resulting from patients’ high expectations and lack of awareness of cost covered by insurance.
- Deficient assessments of the value of some of the new technologies before their acceptance in practice.
- More frequent and greater compensation of victims of disease or injury via malpractice awards, and the associated escalation in liability insurance premiums.
- Inefficiencies stemming from the absence of an organized system of facilities designed to cover the range of needs from elementary care to complex and expensive services.
- Prevalence in the public of self-inflicted illness from substance abuse, violence, and accidents, or possibly self-indulgence or culturally-generated psychosocial stress.
- Inappropriate demands or “medical markets” from lack of sufficient public education to provide self-care for medically trivial events (colds and most headaches) or lack of tolerance for the time and discomfort sometimes required in spontaneous recovery.
For the United States in the 1980’s, the prevailing answer by a society electing conservative governments seems to be just that. Instead of cost containment by rationing care, as occurred with mixed results in Britain’s National Health Service, in this country we are witnessing the organizing of doctors, clinics, hospitals, and medical suppliers into units which have to sell themselves to the public, and thereby have to rely on competition instead of regulation as the principal mechanism of cost-restraint. Major elements of this shift include replacement of conventional insurance and the fee-for-service payment by prepaid enrollment in what are referred to as health maintenance organizations; employment of salaried physicians by such corporations; and reorganization of hospitals, clinics, and equipment suppliers into large units possessing greater command of capital resources and capable of realizing savings through economies of scale.
IV
A small montage of recent issues:
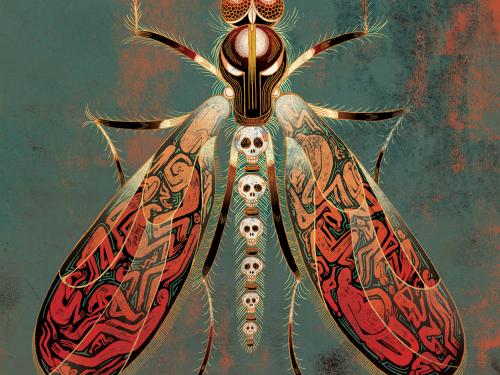
- In 1985 when fear of the acquired immune deficiency syndrome (AIDS) as a result of blood transfusion became marked, some patients avoided coronary bypass operations, some successfully, and others not. Many surgeons then learned to do the operation without using blood, although the convalescent patient then often had enough anemia from blood loss to delay return to vigor during weeks of spontaneous blood regeneration. Which is preferable, the risk of transfusion and quick recovery or the safety and loss of working time in waiting for natural recovery? There is no right or wrong; we will differ.
- In 1986 an expert in liver transplantation hailed the improved 64 percent survival at one year among liver recipients as a reason to relabel the procedure “non-experimental, ” thereby opening the way to obligate insurance companies (and their premium-payers) for the extraordinary costs of these efforts. What should be called “experimental” and funded as research? What should be called a standard practice and funded through insurance? In seeking insurance at minimum cost, how selective can we be in placing ourselves in a “good risk” group in order to avoid the burden of paying for others?
- Members of a state medical society were asked to support a resolution from the American Cancer Society recommending an annual mammogram (procedure for detecting breast cancer) in all women over age 55, who during a subsequent three decades of life may have a 7—10 percent risk of developing that condition. The medical director of a large Health Maintenance Organization—possibly conscious of the extra operating expense involved—spoke against the resolution.
- Reports on formally supervised rehabilitation clinics for patients after heart attacks largely failed to confirm predictions of better survival and activity among participants as compared to members of control groups who regulated their own recovery. Nevertheless, the security, psychological support, and plausibility of such clinics assure their popularity with patients and physicians alike. How much psychological support should we provide, and who should pay for it?
- With lawsuits in progress in several states, a committee of the American Medical Association took the position that in certain conditions of terminal disease and unconsciousness the removal of basic feeding supports is ethically permissible.
V
The name Health Maintenance Organization implies that some of the proposed savings in medical costs can be achieved through the use of more preventive measures and early disease detection techniques among subscribers, services which are frequently omitted from conventional insurance coverage. Efforts to analyze the cost-effectiveness of such preventive screening, however, have been inconclusive or inconsistently positive. The savings realized by HMOs probably derive from a combination of other elements, including salaried physicians, who tend to be more frugal in the use of procedures; economies of scale derived from larger, multipurpose facilities; and subscribers who tend to be self-selected from the “good risk” (meaning relatively disease-free) group of employed, middle-class medical consumers. Large prepaid medical care plans, both nonprofit and increasingly for-profit, have been successfully meeting the needs— ranging from sore throats to open heart surgery—of increasing millions of U.S. subscribers during the past 30 years. Although rumors do circulate of covert rationing of procedures and specialist consultations of HMOs, there has been no evidence of patient neglect as a result of HMOs’ tilting the incentives toward medical savings and away from spending.
There are, however, compromises and risks involved in such plans, and these may increase as more plans come under the ownership of for-profit corporations. Likely problems in the emerging scheme of things include: (a) reduced availability of good medical care for those groups unlikely to enroll in HMOs, primarily again the poor and elderly; (b) for reasons of cost, exclusion from such organizations of training programs for medical students and residents, which have been partly subsidized by government and insurance revenues; and (c) a division of the loyalty of corporation-employed physicians between the interests of their patients and those of the corporation.
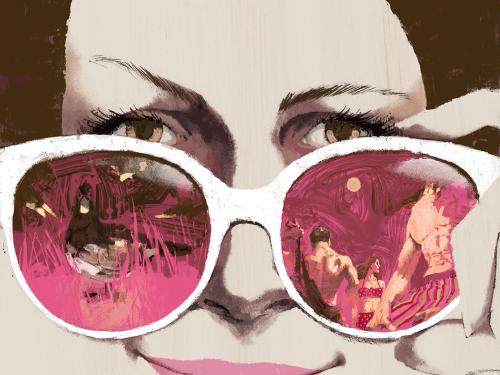
We are already seeing a downgrading of the physician’s image and the medical profession’s cultural authority through increasing use of medical advertising and other competitive, commercial tactics. Some critics can properly assert that doctors’ images have long been too inflated, and that some crumbling of the pedestal is in order. Nevertheless, doctors enter our lives at points of marked vulnerability and uncertainty, death, or major disability. Our need for a trusting relationship then may seem more intense, more significant than our relationship to our banker or lawyer or car mechanic. How will the more modest image of the future doctor affect our capacity to trust him or her in difficult situations? How will this more modest image affect the doctors’ expectations and aspirations for themselves, their tenacity in translating professional idealism into performance?
As more physicians have become corporate employees, there has been a corresponding growth in physician unionization, collective bargaining, and other confrontational tactics, all in an effort to retain professional influence. As Starr has noted, “Profit-making medical schools and hospitals were quite common before 1900, yet both were soon in decline. My argument here is that the profession’s success in establishing its sovereignty in medical care depended on the banishment of profit-making businesses from medical education and hospitals as well as from medical practice itself.” Noted medical economist Rashi Fein has commented, “In the price-competitive market those who would offer more care will lose along with those who need more care. Only the fittest will survive. But the choice of what we mean by “fittest” is still before us. Once our fittest institutions were defined by their activities on behalf of others . . .increasingly fitness is measured by the bottom line on a profit-and-loss statement.” (New England Journal of Medicine, 313, 113:1985)
VI
What we have seen of late in the United States is a heavy reliance on the operation of the “natural laws” of economics to bring about needed corrections in medical inflation. But what we need to see is that the problems of cost, access, and quality of care are inseparable. We need to see also that quality and quantity are not identical, and that a telephone call at night from a concerned physician may be more valuable than an elegant test or operation, In the shift by physicians from dependence on individual pride and responsibility, which is the good part of “professionalism,” to pyramidal organizations of services and facilities, we can attempt to retain quality through vigilant review of clinical charts and compilation of results. No guidelines, review committees, or decision-guiding algorithms, however, will ever identify those special insights and extra efforts that are sometimes the essence of high quality in a physician. In reviewing the partial list of causes of medical inflation given earlier in this essay, we can see that some problems could probably be corrected with minimal impact on quality— excess incentives for procedure performance, deficiencies in technology assessment, Or abuses in malpractice liability mechanisms. We should also see that other causes on the list involve items we cannot or may not want to alter, because we value them to different degrees—the presence of more older people, the benefits of high technology, freedom either to pay for minimizing risks or to adopt risky lifestyles, and maybe a “do-everything” urge. The variety among us in terms of attachment to such cultural values suggests that Americans’ eventual acceptance of uniformity in medical care is only slightly more likely than uniformity in religious affiliation. The use of HMOs, competition and advertising, economies of scale, and a variety of financial incentives and disincentives directed at both doctors and potential patients together constitute a “treatment” directed at only part of the problem. Unless the diagnosis of the problem is expanded to include the larger forces at work in our cultural values, and allowances are made for these in treating our current medical cost inflation, another cycle of revolution and reform in American medicine will not be far off.