Leaving I-81 South in Virginia at Abingdon, just before it dips into Tennessee, the route crawling up, down, and around the Ridge-and-Valley Appalachian Mountains where US-58 heads toward Wise County is blanketed in thick, leafy kudzu vines that engulf just about anything that stands still for long enough: power lines, abandoned garages, even the trees themselves. The gas stations are few and far between; at one just off the highway, a poster in a metal frame near the pumps proudly proclaims virginia is dew country, touting soft drinks the size of a small dog, for a price I could easily pay with the change stashed in my door handle. This part of the Commonwealth might be “Dew Country” compared to elsewhere for all I know, but I felt a wince of shame to see a corporation unabashedly marketing not just soda but this soda in particular, green as cartoon toxic waste, intrinsic to a kind of rural identity. I felt that same wince a day later at the Remote Area Medical free health care clinic each time a dentist hesitantly dropped the expression “Mountain Dew mouth” as a footnote to our conversations about their rural patients.
Once you’re west of Roanoke, one in five Virginians (and one in four kids) lives at or below the federal poverty line—nearly double the state poverty rate—for a total of about 101,000 people. Families of four in this income bracket make less than $24,300 per year; a household of one, $11,880. One person working a full-time minimum-wage job isn’t far above that line, earning about $15,000 per year. That’s low enough for kids in a family to qualify for Medicaid health coverage, but, because the eligibility thresholds for adults and children differ, their parents could easily be out of luck.
An adult with no children, unless disabled, would find themselves falling into what’s been dubbed the health care “coverage gap”: Nearly 33 million Americans—over 10 percent of the country’s population—are without health insurance. Though it’s been at least discussed in the state legislature for the last few years, Virginia is still one of nineteen states refusing federal Medicaid-expansion dollars to close the health care coverage gap for people not poor enough for Medicaid but too poor for anything else. Of those who do qualify for subsidized plans or manage to pay for private health insurance, most will still find themselves trying to scrape together huge out-of-pocket sums for dental or vision services, which are either not covered under basic health care plans or demand high up-front co-pays for common needs like fillings and glasses. And even if one could save enough for treatment, finding local doctors who accept Medicaid is often so challenging that it can seem easier to just give up and work through the pain or self-medicate.
One glimmer in an otherwise dark mountain woods: For the last seventeen years, during the same late-July weekend, an organization known as Remote Area Medical, or RAM, has offered a laundry list of free dental, vision, and medical services. Over the course of three days, at the Wise County Fairgrounds, an all-volunteer staff builds a pop-up clinic—the largest RAM health clinic in the US—from the ground up, and serves more than 2,000 patients from more than fifteen different states. All told—adding up doctors, nurses, and general support staff over the weekend—the patient-to-volunteer ratio ends up at about one-to-two.
As I pull up to the fairgrounds, dozens of rows of cars glint to nearly the horizon—patients’ vehicles in one field, volunteers’ in another. Those seeking care are given entry numbers based on the order in which they arrive, and can’t leave without forfeiting their place, so many make plans to camp out for as long as two days before the gates even open—sleeping in their cars, in tents, or on the ground, to make sure they snag a low number. You’ve seen the photos of people in pup tents in line to buy Hamilton tickets or a newly released iPhone? It’s like that, but instead of paying $200 to $800 to hear a rap about Yorktown, these campers are hoping to get cavities filled, lungs x-rayed, and new pairs of glasses made—for free.
RAM was founded in 1985 by Stan Brock, a British philanthropist, actor, author, naturalist, cowboy, and the former cohost of Mutual of Omaha’s Wild Kingdom. A boarding-school dropout, Brock traveled at age sixteen from England to what was then British Guiana, where he began his stint as a vaquero, at times in remote parts of the rain forest near the Brazilian border. After a particularly brutal mishap with the side of a corral and a wild horse called “Kang,” which he had been attempting to tame (he casually recalls: “Kang had already killed two people, and I was number three on his list”), Brock realized that he was an almost impossible distance from the nearest doctor. “As a result, I came to the conclusion that at some point, we needed to bring doctors closer to people than twenty-six days on foot.”
Years later, after adding airplane pilot to his list of occupations, Brock began organizing medical-relief missions to British Guiana, to remote mountain areas of Mexico, and, eventually—after running low on plane fuel and making an unplanned landing in Tennessee—the rural American South. He established the RAM head office, in which he makes his home, in Knoxville. “It seemed like a nice place to be, nice people. And they asked me to do some public-service announcements for the Knoxville zoo,” he says. Once he got his bearings in his new hometown, Brock found that “remote” didn’t just apply to developing nations—it also described his own backyard. And it was a big backyard.
Even at eighty, Brock has the presence of an action hero and gentleman: part Edmund Hillary, part Alec Guinness, part “Crocodile” Dundee. His commitment to the RAM mission is total: He has no assets, no personal entanglements, and no regular activities outside those of the organization. He sleeps on a mat on the floor of his office, exercises every day, and manages and works at nearly all of the clinics—a dedication that comes across as monkish, but styled in a khaki safari jumpsuit and baseball cap, complete with the RAM logo.
RAM is one man’s vision, but as an organization it’s more complex: a 501(c)(3) nonprofit funded entirely through private donations, both corporate and individual, and—except for a small, paid staff—completely dependent upon thousands of volunteers for everything from performing oral surgery to making baggies of Cheerios to hand out to patients’ toddlers. Corporations and wealthy patrons have donated EKG machines, autoclaves, RVs, and even airplanes. In addition to international and disaster-relief missions—RAM provided help after the earthquake in Haiti in 2010, and set up a clinic using space at the New Orleans zoo a few months after Hurricane Katrina—the group has held 809 general health-clinic events across twelve states throughout the Southern and Southwestern United States. Over the last five or six years, it added urban stops such as Los Angeles, Chicago, and, in 2015, Anaheim, California, to its regular locations, knowing that while cities aren’t remote, the opportunity to receive health care within them often is.
By 3:30 a.m. on Friday morning of the Wise clinic weekend, volunteers with flashlights are moving from car to tent to car in the patient lot, handing out admission numbers for the day. By the time the sun rises at 6 a.m., they have given out 1,600 slips of paper that will serve as golden tickets to the clinic. On Saturday morning, they will give out about 600 more.
I first meet Sheila Harris, a fifty-eight-year-old former paralegal, in the early hours of the opening day. Sheila has worked her whole life, but steady legal work became a hodgepodge of whatever one-off odd jobs she could find after the birth of the last two of her six kids, and she now earns only a small income taking care of children in her home. She’s one of the first hundred allowed through the gates, leaving hundreds still packed outside the fairgrounds’ fences waiting to hear their numbers through the megaphone.
Sheila, her daughter Amy, her sister Cindy, Cindy’s daughter Elizabeth, and four other family members have traveled about three hours—in two cars—from Wytheville, Virginia, to arrive at Wise two days early. Amy has her two-year-old son, Parker, with her, because she wasn’t able to secure child care for the days she’d be away from home. Eight adults and a toddler, they would end up sleeping in the two cars for four days, in a field of strangers sleeping right next to them. During the first couple of nights, they would drape blankets over the windows for privacy, but would take them down after it made the cars too hot to sit in, much less sleep. It is everyone’s first time at the clinic, excepting Cindy, who’s been twice before and is the ringleader of the group on this trip. Once, she says, she arrived early enough to be the very first patient served. “It was still a long couple days, though.”
Cindy is at RAM this year to get new eyeglasses and to support her twenty-nine-year-old daughter Elizabeth, who needs glasses too, as well as the extraction of two molars. Elizabeth also hopes to get a partial denture plate. She took a bad fall a couple years ago and broke her top front teeth, most of which have been completely missing for years. At the time of her fall, she’d had decent health insurance, but still had to pay $1,000 out-of-pocket just to rebuild one tooth, which later cracked again anyway. Cindy and Elizabeth are currently both receiving disability benefits—essentially their only source of income. Without RAM, a new pair of glasses with a current prescription would be a luxury item for either of them.
Sheila needs glasses as well, but is first set to have six teeth removed—a couple of which are already in pieces—and upper dentures made and fitted. Neither Sheila nor Elizabeth will smile open-mouthed. They haven’t smiled that way for years, in fact, out of embarrassment. “I guess I’ve kind of withdrawn from people because of it,” Sheila says. “I used to talk to anyone, anywhere, about anything—real outgoing—but I haven’t been like that in a long time.” Smiles or not, I’m amazed they’re talking to me—a stranger, “the press” as they jokingly refer to me—and I’m humbled by their openness and good humor, these women who’ve so far spent a day and a mostly sleepless night in a blanket-covered van just to wake up and have major oral surgery. Sheila pulls a roll of TUMS from her shorts pocket and says it’s the only thing she’s been able to eat since the day before, on account of her nerves. She’s brought the broken crown with her “in case they can use it or something,” and holds it tightly, the way I might hold $1,000.
It is still dark when the whole family completes registration in the triage tents, where nurses take their basic information and vitals and start patient charts for the various services they’ll receive: pink charts for dental, blue for vision, white for medical. “Pink gums, blue eyes, white coats,” veteran volunteers always tell the newbies. At every RAM clinic, most people need dental work, which is usually prioritized over other care because of the time and intensity of the procedures. Some patients, though, don’t make it very far past triage: If their blood sugar or blood pressure is too high, they get pulled into another tent, where trauma doctors examine them again and try to bring the levels down. The trauma tent is where a couple dozen patients each year at Wise first learn they have untreated diabetes.
It is cool outside before sunrise, but will reach a humid ninety-five degrees by late morning, and get even hotter by Saturday. There is no misting tent—a common amenity at hot, summer festivals—and no air-conditioned space except for the mammogram and radiology RVs—a feature RAM hopes will attract patients to those services, if nothing else. Volunteers drive Gator utility vehicles back and forth across the fairgrounds all day, handing out cold water and chilled neck wraps. All the outdoor waiting areas collect patients in tight rows on metal folding chairs—the scene resembling a kind of yearbook photo of need—and the sheer volume of elderly folks and patients with visible disabilities is striking. I worry how they will endure all the heat and walking. A dozen empty wheelchairs are stashed near the entrance; just eight or so hours later, there are only two left.
The Wise clinic is still RAM’s largest event each year—measured by both number of patients and volunteers—thanks to a dynamo known simply as Sister Bernie. Sister Bernie Kenny of the Medical Missionaries of Mary is a nurse-practitioner who has been dedicated to serving Appalachia since 1978. She started out with nothing but her credentials and a red 1968 Volkswagen Beetle that she used to drive up through the hills and hollers of Southwest Virginia to connect with the people living tucked into them and deliver whatever health care services she could. After a few years and past the life span of her car, she managed to create what’s now known as the “Health Wagon,” a dozen or so nurses and staff who serve twelve rural Virginia communities via a renovated RV and a 4,900-square-foot stationary clinic in Wise.
In the early days, though, Sister Bernie found one particular problem, time and again, that she just couldn’t address from her car: “We were every week seeing people with dental abscess—we’d give them some antibiotics and a week later, the same person would be back, because we couldn’t get them any dental care.” A missionary on a mission, Kenny traveled some seventy-five miles to Mountain City, Tennessee, where she’d heard that an Englishman named Stan Brock was holding an outdoor health clinic. She brought him his favorite apricot juice and suggested RAM come to Virginia. “Oh, he’s a prince of a gentleman!” she says of Brock. Whether it was Kenny’s charm, or the apricot juice, RAM Wise came to Virginia in 1999. In the years that followed, it spread to other smaller rural counties across the state, thanks in large part to their partnership.
In my wanderings over the course of the clinic weekend, I catch Kenny working in just about every corner of the place, dressed not in the habit her name conjures up, but in pink seersucker scrubs with anchors embroidered across the shirt. Usually when I spot her, she’s chatting up patients and volunteers, her heavy Boston accent somehow braiding smoothly with the drawl of locals, exemplifying the high standard for compassion that seems to make RAM tick. It emerges over the course of the weekend as a theme. Every patient and volunteer I speak with articulates some version of this feeling that neither government nor private care has been able to replicate: RAM is trusted because everyone involved operates from a place of kindness, dignity, and respect that doesn’t seem to exist in traditional health care venues. A decent number of the clinic volunteers started out as patients; once they received care, they wanted to help give back to others.
“They treat you like you’re special,” Sandra says when I ask her why she came to the clinic for help. Sandra has worked at a Tennessee manufacturing plant for thirty-eight years, surviving several layoffs that many of her friends did not, but her company-provided health insurance doesn’t cover dental care. She previously funneled most of her pay toward caring for her husband, who recently passed away, and who after a cancer diagnosis and a heart attack was not disabled enough to receive benefits but required a lot from Sandra, both financially and emotionally. Since his death, she says, her grief has brought on a good deal of depression. She’s here at the clinic for an extraction and a filling. “These are nice people,” she says. “And they act like you’re somebody.”
Though traffic through the medical stations is steady—usually with primary exams helping to direct patients to specialists like endocrinologists—the main attractions of every RAM clinic are the dental and vision-care services. Wise sets up about eighty mobile dental stations outside in a grid under large fair tents—one section of tents reserved for cleanings by hygienists, a second block for fillings, and, in the back tent, four or five long rows of stations for extractions. The vision and medical services are each delivered in two large barns (the makeshift exam rooms are jerry-rigged livestock stalls, with bedsheets hung for privacy). Specialized services such as x-rays, mammograms, and orthopedics are provided in converted eighteen-wheelers or RVs. Other informational and preventive-care tents (treatment for substance abuse, smoking-cessation counseling, and mental-health care), clothing and book donations, snack and water stations, and a pharmacy are scattered wide across the grounds. The only bathrooms—for patients and volunteers—are several dozen porta-potties mixed into the layout. The full Wise clinic footprint is see-it-to-believe-itimmense: One general-support volunteer working as a patient escort could easily walk fifteen miles or more in a day while traveling back and forth between service areas.
Other such RAM clinics may be smaller, but they operate under similar conditions. The Smyth County, Virginia, clinic is set up on the tarmac and in emptied hangars of the local airport; services there must shut down at a particular time so that planes can be moved back inside. Another clinic, in Virginia’s Northern Neck, finds its home for the weekend in an elementary school. One Tennessee event is held right on the Bristol Motor Speedway infield; Brock can often be seen on the track on his bicycle, vigorously pedaling angled laps.
The dental stations alone are their own kind of wonder. Each dental chair, tool station, and lamp arrives in folded parts in a heavy bag or case. They’re hauled off trucks, unpacked, and assembled by several dozen dental-student volunteers who will spend the weekend assisting the dentists and later reverse the setup process, reloading everything onto the trucks. Within the dental tents are 1,600 feet of electrical lines running 240-volt three-phase electricity to each chair from the fairgrounds’ power; a jackhammer compressor to power the air lines; 500 feet of trunk line; and hundreds more feet of white PVC pipe that snakes in a grid through the rows to deliver suction, via a dry pump, to each of the eighty stations—one chair every six-and-a-half feet.
And there’s no getting around it: Medical services create medical waste. Every four to five hours, no matter where patients may be in the process, the whole dental operation powers down and comes to a halt for ten minutes while two steel hazardous-waste tanks are emptied into designated porta-potties to be hauled off and dumped later.
While kudzu is the protagonist of the Southwest Virginia landscape, teeth play the starring role in the judgment of its people. “Poor teeth, I knew, beget not just shame but more poorness,” writes Sarah Smarsh in her 2014 Aeon essay on class and dental hygiene. It’s easy to imagine that a designer costuming a poor, rural Southern character in a movie would likely think to begin by styling her teeth, not her clothes. But that kind of judgment is not just fiction: Shame, poverty, and the verb beget are at the rotten root of what brings people to RAM clinics. Poverty begets depression and anxiety. Shame begets avoidance. Poor nutrition begets decay. A dearth of doctors and dentists begets poor preventive care. Pain begets self-medication. And it’s cyclical: Missing teeth beget unemployment, begets missing teeth.
One woman sitting near Sheila and her family in Extraction Row says she’s recently been fired from a waitressing job after losing a couple of her front teeth. Her manager didn’t want her in front of customers. Food service has made up the entirety of her employment history, and she’s having trouble getting hired permanently elsewhere for similar reasons. Even when she was working, she says, she couldn’t afford the cost or time-off necessary to treat her teeth—or anything else, for that matter. The RAM clinic, once a year, is her sole source of health care. She now works as a temp in one of the many call centers planted in Southwest Virginia.
Dr. Joe Smiddy, one of the longtime volunteer doctors on-site, has seen similar scenarios play out for patients here, time and again: “Once they lose their teeth, or they have unsightly teeth, they lose part of their own marketability. They have trouble finding a job,” he says. “ ’Course when they lose their job, they lose any health care they might’ve had. And then you can have substance issues where people are self-medicating with tobacco and street drugs for what is real pain and real anxiety.”
Poverty also begets limited choices. Sugar provides a cheap and legal high—from endorphins—and caffeine does the same with energy. Both can be used to self-medicate and as an easy way to make your kids happy when you can’t afford much else—perhaps especially when you have to bring the whole family to the grocery store with you and have wide eyes looking up at you, pleading with you for a treat. I look over at Amy’s son, Parker, a little grumpy from having slept on the bench seat of his grandmother’s van, and think, I’d give him a cookie, too.
Terry Dickinson, another mainstay at RAM clinics, is the executive director of the Virginia Dental Association and the founder of Missions of Mercy, an organization of all-volunteer dental-health care providers who treat uninsured and indigent patients at two of the in-state RAM clinics, including Wise, in addition to conducting their own charity dental clinics. From Dickinson’s view, “the economics of this community are such that when they go to the grocery store and buy food, it so happens they get a lot more food when they buy highly processed, high-carbohydrate foods, and, instead of water, they pick soda pop or sports drinks, or any of that stuff that’s just as cheap.” Nearly 100,000 people in Southwest Virginia receive Supplemental Nutrition Assistance Program (SNAP) benefits (formerly known as “food stamps”); a family of four receives $115 per week on average for food, or just about sixteen dollars per day. And unhealthy processed foods aren’t just cheaper: They don’t spoil as quickly, and they can take less time and fewer ingredients to prepare.
But is all this really endemic to Appalachia? “I think they want pretty white teeth just like everybody else,” says Dickinson. “And you’ll see poor dental health everywhere in the state—you’ll see it in the Eastern Shore; you’ll see it in Emporia; you’ll see it in Suffolk; and you’ll see it in the middle of Fairfax County. What you want for everyone is personal responsibility, but you’ve got to give people the education and tools they need to make those decisions.” And, he says, for people living in poverty, “we just haven’t done a good job of that. These are people in survival mode.”
Living in survival mode means prioritizing where you spend your limited income. There is no discretionary fund. A 2015 survey conducted by the Federal Reserve Board to determine what practical effects, if any, the economic recovery was having on families found that 46 percent of Americans did not have enough money on hand to cover an unexpected $400 expense. When that expense is a medical emergency, it often leaves only two options: Use a credit card if you have one, or forgo care until the pain aches well past emergency and reaches unbearable. A recent study of two surveys commissioned by Demos—a public-policy group—by analyst Sean McElwee found that dental expenses were the most commonly cited contributor to high credit-card debt, with doctor visits, prescription purchases, and emergency-room visits not far behind. And among households that already owed medical debt to credit companies, 63 percent reported “either postponing or not filling a prescription, not visiting a doctor, or skipping tests, treatments or follow-ups.”
Dickinson tells me a story of one of his former RAM patients that hits this point even harder: “I remember this young lady that needed some complicated stuff done, and so I talked to a friend of mine who’s a specialist down in Abingdon, and I said ‘If she can get there, would you take care of her for me?’ And he said sure. Well, she says, ‘I’d have to check with my husband’s parents, because we don’t have a car.’ There’s only one car for the whole family—one car.” He holds up one finger and pauses for a second. “And so for her to commit to going from Wise to Abingdon—gas, time, other family members’ priorities—it’s not going to happen. And nobody thinks about that. People who don’t know that world don’t think like that.”
At registration, RAM volunteers don’t ask patients for their ID, their income, proof of insurance, or their citizenship status (which can be especially important for the clinics on the Northern Neck of Virginia, where many migrant-farmworker camps are based). They do try to get good contact information—whether that’s an address, an e-mail, or just the phone number of a friend who can find them if need be—so that there’s a way to provide necessary referrals or follow-up care. They also try to take as accurate a basic medical history as they can, though the triage nurses say that some patients can’t recall ever going to a doctor, even as children.
Putting stock in a long-term investment like one’s health requires hope. Embedded in preventive and rehabilitative care is the presumption of a long, fulfilling life. Health insurance is an invisible protection—it doesn’t nourish a hungry stomach, or power a refrigerator, or fill a gas tank. People who don’t know that world don’t think like that.
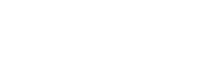
Sheila is in Dr. Dan Laskin’s dental chair and is about to have her extractions done. There are picks, forceps, syringes, and what looks like a hammer and small chisel on the tray beside her. Even when you’re having six teeth pulled, if your dental care is happening under a tent at a fairgrounds, you’re given some lidocaine and a few large, well-placed shots of novocaine, but you don’t get much more of an anesthetic cushion than that. The procedure is likely as smooth as it could be, though Sheila moans and wriggles often from the pressure. The dental assistant gets her to close her eyes and talks her through some visualization strategies involving her favorite place: the beach. Still, it only takes about thirty to forty-five minutes before her mouth is packed, and the experts are ready for whoever’s next. Numbed and frazzled, Sheila says to Laskin through the gauze, “You are freaking amazing!” and hugs him.
Elizabeth has already had her two extractions done, and is now at the dentures station, where another dentist has inserted a tray of alginate paste into her mouth that will become the mold they’ll use to make her partial plate. The dentist has to keep the tray pressed tight against Elizabeth’s swollen, sore jaw for a good minute, but afterward she says she didn’t mind it too much. “It was easier than getting my teeth yanked out!” She heads over to the vision section to get in the long line for glasses.
What’s quickly apparent in observing this organization (that sometimes seems more like a carnival than a hospital) is that the doctors are as compelling as the patients. Smiddy is a seventy-four-year-old retired pulmonologist, now a full-time medical volunteer, who grew up in Wise, the grandson of a coal miner. He got his commercial driver’s license in order to drive the eighteen-wheeler rig that holds his mobile x-ray office to RAM clinics. Sometimes, during a lull in patients, you can catch him picking a banjo in the clinic bluegrass band he’s pulled together with a few regular volunteers. Smiddy has seen it all: Most of what he has to share with me begins with “And I can say this because I’m from here.” When he talks about Appalachia—whether he’s speaking of the patients living in poverty or the doctors who treat them—it’s evident that these aren’t just hispeople; he is theirs.
“The people of Southwest Virginia,” he advises me, “are self-reliant, and their self-reliance and their love for their people and their land is such a wonderful thing, but it’s also what holds them here. There’s a social importance to people who are from here being really glued here. So why would we move to another part of Virginia? Why wouldn’t we move to where the jobs are? But we’re totally averse to doing that, and so we have a large population who live in an economically deprived area. The schools are struggling. The churches are struggling. Every time they build a Walmart, it puts several mom-and-pop stores out of business. Your barbershop’s gone because you get your hair cut at Walmart, your beauty shop, your auto-repair—everything Walmart. And then you’ve got people working at Walmart who don’t have health insurance, either.”
People not in poverty often ask those who are to movein various ways—off of street corners when they’re homeless, away from their depressed hometowns when they’re unemployed. They’re asked to move couches off of front porches and cars off of blocks. Politically, they’re usually asked to move out of their own way.
All of the qualities that Smiddy describes, though, are what most people would likely say they want in a healthy community. We want people to help take care of their parents when they get older. We want grandparents to be able to step in and help with their grandkids when it’s needed. We want people to love and care about their land and neighborhoods and to know one another. We want a shared history, vibrant cooperation. These are all characteristics we celebrate, it seems, everywhere but communities of poverty. In places like Southwest Virginia, we don’t honor these relationships, underwrite them—socially or financially—in the same way we do in middle-class or affluent regions. Instead, what we cosign as a nation, as a matter of policy and entertainment, are the rural stereotypes, to the point where it’s become gray as ash where the photo op ends and the reality begins.
For decades, people in rural Appalachia have also been asked to move mountains. In his mobile rig, Smiddy will x-ray “just about anything you can put in front of the machine.” He mostly looks at lungs, though. “We’re a belt of lung disease,” he says. “Southwest Virginia is a belt of asthma, COPD, emphysema, and, of course, heart attacks, strokes, and diabetes. Part of that is smoking—we in Southwest Virginia have a tradition of starting smoking at an early age. There are towns where the average age of starting smoking for current lung patients was age ten.” But part of it, he says, is the coal dust and environmental allergens. When business was booming, coal workers were paid well and offered decent health insurance, but layoffs and facility closures, especially those by Alpha Natural Resources in recent years, have left many in the region with poor health and poorer prospects for work and the health care coverage that used to come with it.
So if long-term health requires hope, what does hope require? At some of the smaller RAM clinics held in nearby Southwest Virginia, like Lee County and the town of Grundy—two of the poorest localities in the state—where patients are mostly local, Dickinson says, they’re starting to see a difference. Intake numbers are dropping slightly because, he thinks, the services are working to stem chronic needs, and even the small step of having patients return once a year is improving their health. His goal for Missions of Mercy isn’t just measured in the number of pop-up patients seen or served, but in leaving a footprint of sustainability in the communities they go through. “You get depressed after a while,” he says, “because it’s just so overwhelming. But you have to start somewhere.”
Patients in need of follow-up care are referred to local dentists, who are cultivated to offer their services to indigent patients during RAM’s 362-day off-season. Still, “at some point in time, you just need to stop the disease,” he says. “We’re doing better at it now, but we could just do so much more. The educational aspect of it, nutrition, school nutrition. It’s not that they’re ignorant people. It’s that they don’t have the money to buy the food that doesn’t hurt you, or the education of why you need it.”
What they also don’t have are good-paying jobs with accompanying health insurance. “All of the politicians are singing this little fairy tale that coal is coming back,” Smiddy says. “They’re living in that fairy tale, and so what they’re not doing is accepting the reality that we could plan, we could think ahead. We could reach broadly to incorporate everybody—schools, churches, civic organizations, mayors, community leaders—that we all pull back together and say, ‘We have a goal, and our goal is we’re going to try to predict as best as we can the jobs of the future, and we’re going to start now.’ I don’t mean to be ugly when I say that there may be some people who will miss that curve, but we could build for their children.”
Coal is complicated in Appalachia. The coal industry has torn up pieces of Southwest Virginia and the bodies of those who’ve mined it, but as it has declined here, the men and women it employed—many of whom have high-school degrees at most—have slipped from relying on steady middle- and upper-income salaries to prospecting for minimum wage. The classified ads in places like Wise and Coeburn, Virginia, are thin and advertise for positions like “Customer Service Representative 1” and “Cashier (Part Time).” We may be able to replace coal with other comparable energy sources, but we haven’t yet prioritized how to comparably replace coal jobs.
“I mean, how many call centers can you put down here?” Dickinson says. All people want here, he repeats, is a good-paying job.
Saturday. All eight of Sheila Harris’s brood have now spent four days and three nights living in two cars. They’ve had to stay this long to wait for their glasses and partial dentures to be finished. Parker got to spend Friday night indoors with Amy at a nearby friend’s house, but the two are back out in the unforgiving heat and humidity for the day.
Sheila decides to get a pap smear and a mammogram while she’s waiting for her bifocals to be made; lenses are made on-site in yet another RV. From Friday morning until Sunday afternoon, volunteers—some of whom have just been trained—measure and cut prescription lenses for almost 650 pairs of glasses.
Cindy and Amy walk over to a large tent where a few thousand brand-new frames, all donated, are set out on long folding tables so that patients can select the styles they like. It’s an impressive spread. A few scattered regular volunteers help consult on shape and fit. Amy browses and says she’s decided to get new glasses today, too—she might as well since she’s already here. Last year she shelled out $1,000 for two pairs for her husband, counting the cost of optometrist visits, lenses, and frames—and they even got them at Walmart, she adds.
The barn where the vision exams are given is a touch cooler than outside, mostly because the room has to be kept dark for the testing. The majority of patients here are getting basic checkups and prescriptions written or updated, but occasionally—as with the dentists—the optometrists diagnose more serious health issues: glaucoma, cataracts, macular degeneration, diabetes. One patient at a recent Smyth County clinic had to be rushed to a local ER, due to an optic-nerve issue that could’ve quickly led to a stroke. Quite a few patients find out that they have some kind of eye condition for the first time while here, and not just the serious diseases. Prior to their exams, some don’t even realize they need glasses.
Dr. Victoria Molnar Weiss is the optometrist who runs all the Virginia RAM vision clinics. Her current patient, Steve, looks at a chart projected onto the wall and says, “Well, the first letter is A?” The glasses he showed up with have a prescription from 1994, which would be tough enough, but Steve also just learned he has uncontrolled diabetes—his glucose measured 332 mg/dL at triage. “When your body’s shot,” he says, “you get depressed.” That cycle, he says, makes it even tougher to get healthy, even when you want to. He promises Weiss he’ll walk down and see the endocrinologist over in medical.
Weiss and the other eight or nine volunteer optometrists and ophthalmologists will see one third of the 2,200 patients coming through the Wise clinic over the weekend. She explains that the ability to get new glasses can be the lure that first brings patients to the clinics, and then, over time, their trust grows. “The patients see us up at 3 a.m. too, so it kind of helps them feel like we’re all in this together,” she says.
What also helps is the ability to use the money they might otherwise have spent on frames, lenses, and an eye exam on other necessities. People living in poverty are often playing a kind of shell game with whatever limited income they have: Skipping a power bill to pay for a visit to the eye doctor might work for a month, but it could put them behind for a year. Much easier to keep using old lenses, squint a little harder, and live through the migraines.
Elizabeth’s “partial” is finally ready. The dental tech is fitting it for her, trading it in and out of her mouth in between filing her teeth down to eventually arrive at the best fit. After a few revisions, they’re both satisfied. The tech doesn’t have a mirror, but holds up her iPhone with a forward-facing camera so Elizabeth can see herself. She has front teeth for the first time in years. She both smiles and tries not to at the same time. She is now crying. Her mother, Cindy, is crying. The dental tech and I are both crying as we watch mother and daughter cry and hug each other.
Elizabeth hugs me even, and says, “It doesn’t feel normal to smile. It feels weird.” I think about a bad fall of my own, several years ago, that knocked out one of my incisors. It happened on a Friday. I scheduled an emergency dental visit that Saturday, and by the time my coworkers saw me on Monday morning, I had a high-quality temporary crown in place. No one would ever know I was missing a tooth unless I told them. I think about that glass-house veneer of perfection that money and privilege create. Sometimes the opposite of poverty is privacy.
By Saturday evening, the whole family has gotten just about everything they came for: glasses, extractions, dentures, and even a few bags of clothes and shoes from the donations tent. They’re nearly packed up when Sheila discovers her van won’t start. She seems much less worried than I would be, and I come to learn it’s because this has happened multiple times before—she knows how to fix it herself, she says. She crawls underneath the van and reattaches a loose wire, and when she tries it, the engine turns over.
Late morning on Sunday, I finally catch up with Sister Bernie just as the clinic is closing down. “Today we had a young woman, twenty-seven years old, who had all her teeth out,” she says straight away, before I can say a word past “Hello.” “And her hope for dentures is 2018. How can she live? How can her self-esteem, or her nutrition, or her hope of ever getting a job? It saddens me. But the wonder of being here is all these volunteers with one purpose: to help one another. All denominations, all faiths, all colors, everybody together, and we get energy one from another.”
I ask her what she would do if I gave her a magic wand that she could wave and change one thing for the patients here at RAM. She gives a version of the same answer all the nurses and doctors and most of the patients give when I ask them: “Everybody has the right to health care—it’s not a privilege,” she says. “Your neighbor’s health affects you, so you want the best for your neighbor as well as yourself.”
Sister Bernie, like all the nurses and doctors and patients, says that dental and vision coverage need to be included in basic health-care policies—especially when the root of a major health problem or disease can literally start at the tooth. Consider this: Someone living in poverty with no health insurance gets a toothache, but swallows the pain for months, because what else is there to do? She finally tries the ER when it gets too bad to eat, sleep, or work. She sees a nurse or a doctor, but not a dentist, so the actual cause of the pain stays untreated. The ER doc gives her some antibiotics and maybe some prescription pain medications. She uses up the prescription and then maybe looks for something cheaper on the street to dull the pain, because the tooth is never fixed. No one I speak with mentions heroin or methamphetamine by name—it’s always just “street drugs.” In the meantime, the abscessed tooth could go septic and turn just as deadly as an overdose.
Sister Bernie sees this repeatedly, across generations of families. “But the people who come to RAM want to be healthy,” she says. “A lot of them don’t take vacations, or can’t. They come here.”
One patient I met started off from her house two days before the clinic opened, walked twenty-seven miles to Wise just to have a couple teeth pulled, then walked twenty-seven miles back. Elizabeth started with a partial denture that gave her back her open-mouthed smile—and maybe some confidence. Each of the RAM dentists and doctors and nurses and support volunteers started with a weekend of their lives: offering up their time, their skills, and their compassion to thousands of people they didn’t know who had needs they couldn’t completely address.
Stan Brock started with a concussion and an idea about how to bridge a twenty-six-day-long distance. Access to health care is about more than just reducing the travel time between patients and doctors—it’s about bringing down those intangible barriers that make a distance seem impossible to cross. The stereotypes that teach that people living in poverty get what they deserve, choose their own poisons, dig their own graves; the employment barriers that leave medical and dental students with a mortgage worth of school debt, such that they can’t afford to treat folks who can’t afford to come to them for care. RAM doesn’t solve and won’t solve the US health care crisis—or poverty, for that matter—but it clears a path. One that starts right in our own backyards.
3 Comments
with these hands - Art of caring
Beautifully written--my wife and I are physicians and we intend to volunteer with this wonderful organization.
Thank you to each of you. I just read this today. You each did a wonderful job on this perceptive piece. I know well all the main parties mentioned and have volunteered with the Wise RAM and a few others in the coalfields over these years. You certainly captured it essence and breathe and the profound respect and goodness of Stan, Bernie, Joe et al. You also were very faithful to their calls for universal health care. All in all, you made what was already a story, a better story. Well worth the retelling. Thank you and Happy Easter.