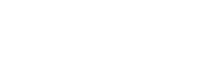
My son suffered a gruesome injury at the beginning of summer—on the last day of school, just a few minutes before I picked him up from a get-together with his rat pack of middle-school pals. Tag in the woods behind the house, night coming on. Tripped on a root along the path, fell head-first onto the jagged end of a fallen branch. Scalped himself along the temple, like a cocktail napkin folded corner to corner, barely missing his eye. Just shy of thirty stitches.
We arrived at the emergency room around 8:45 p.m. I was composed for an hour or so, and then the waiting started to wear me down, and I became less and less a stabilizing force. Pacing, huffing, flagging down anyone in scrubs. He was, after all, a child with a pretty serious head injury, covered in blood, at a premier pediatric hospital. My wife, of much greater mettle than I am when it comes to injuries, especially bloody ones, arrived and took over, sending me home to be with our daughter and wait for news.
A nurse finally led my family down a crowded hallway and into a room where they spent agonizing hours watching doctors and nurses dart past—clearly fried, understaffed, on heroic autopilot—with no answers or much attention to offer a kid with a gash on his head until, deep into the next morning, a resident came in to perform the fraught and delicate task of suturing our boy’s face. Over the course of another torturous hour, our son pumped with as much pain killer as his mother would allow, this extraordinary doctor leaned into her training and steel nerves and sewed him up. He was home by 4:30 in the morning.
Every scar has a story. There’s a cathartic release in telling it, and certainly an easy empathy between listener and teller, since the listener often has a scar story of their own. We find communion in scar stories because they are, after all, stories of endurance where the trauma has been tamed, even if just a little, by the telling.
Hospital stories—and by extension, health-care stories—are another matter. They evoke less a feeling of communion than commiseration, without much of an upside: some bitter memory of feeling helpless against a suffocating bureaucracy or byzantine system, against time itself. Far from uplifting, health-care stories tend to arrive at the same cautionary tale: Ours is the greatest health-care system in the world, but the foundation has cracked, and the cracks are spreading, and no one can do anything about it.
This problem extends well beyond the emergency room and into the humblest of family practices. No one working in medicine is immune to the pressures of this broken industry. I hear it in the exasperation at the front desk of my own doctor’s office, in the nurse’s sighs as she draws blood. I see it in my doctor’s bearing—let’s call him K, a nod to his Kafkaesque circumstances—as he struggles to talk with me at length while being obligated to check boxes on his screen.
Doctors are often on the receiving end of our frustrations with health care, but it’s irrefutable that an increasing number of them are feeling equally powerless, equally vulnerable. As Emily Silverman, a physician-writer who wrote the reported feature, “Best Practices,” for this issue put it to me: “When patients encounter the system, it’s easy to see doctors as the face of that system and to assume that the doctor and that system are one. And there’s some truth to that, but it’s also true that doctors are suffering.” The consequences are unmistakable. As Silverman points out in her story, a 2023 survey of physicians found that 70 percent of them wouldn’t recommend a career in medicine. “In short,” Silverman writes, “medicine is facing an existential crisis.”
She should know. In 2022, she took a step back from medicine after suffering from burnout. The conditions for that burnout preceded the pandemic, of course, as overburdened hospitals drove many doctors toward a professional madness that only intensified with the rise in COVID-19 cases. For many of them, leaving medicine was a matter of self-preservation.
But even before the pandemic, doctors fed up with the dehumanizing structures of the health-care industry were seeking ways to free themselves from it. One alternative, which is the focus of Silverman’s article, is known as direct primary care (DPC), wherein patients pay a monthly fee for essentially unlimited access to their primary-care doctor, to address anything from a cold to anxiety to, in some cases, a broken leg. Silverman guides us through the history of this quixotic revolution in medicine, talking with patients and doctors about how and why it works, and why it’s so difficult to scale up. Whether it’s the inflexibility of insurance companies or tax laws that prevent it from being more affordable, DPC has enormous obstacles to overcome in order to effect anything close to widespread change. At best, it’s a revolution taking place in small communities, in fits and starts. But where it does work, Silverman says, the outcomes—for both patients and doctors—offer insight into just how profound its potential can be. “Good care heals both parties,” she said. “The healing comes from the space between—from the art of the encounter.”
I asked K if he had ever considered striking out on his own with the DPC model. Though his practice operates under a conventional health-care management company, his actual style of practice incorporates many of the same principles as DPC. Part of the reason he seems to be under so much pressure, in fact, is his insistence on spending time with patients—not just in order to listen but to educate them about making smart choices toward better health.
“My brother sees thirty to forty patients a day,” he told me. “He does really well financially. And I’ve told him about the different avenues of health I take with my patients, whether it’s nutrition, exercise, sleep, spirituality, what they’re doing for their endocrine systems—the time you have to spend talking to educate them about the causes of disease. He was like, ‘You’re insane. There’s no way I can talk to my patients about this. I don’t know how you do it.’ The way I do it is I see fifteen to twenty patients a day and work paycheck to paycheck—or not even.”
In many ways, K seems like the perfect candidate for DPC, since his ethos under a traditional corporate structure leaves him stretched so thin. But he’s skeptical about DPC’s potential without any radical overhaul of the tax code or, more to the point, a fundamental shift in American health culture. Thirty to forty patients a day was just a symptom of a shortsighted system that, as he put it, “very much favors lifespan over healthspan. Sure, we can keep people alive longer, but are they truly thriving and are they truly feeling well? The answer to that is an absolute no.” K had much to say about the intricacies of the health-care castle, its knotted intractability and counterintuitive bottom lines. Ultimately, he argued, accountability for a better health system stretched from insurance CEOs to patients themselves.
Listening to him, I realized how much we had in common, just two dads kvetching about things that didn’t work, about paying the bills. And I think back now to when the pandemic unlocked the realization for many that, despite their power and incredible capacity, simply put, doctors are people too. The toll of serving on health care’s front lines became intensely clear then. And while the pandemic may have subsided, the system is arguably more battered than ever, under unrelenting pressure.
Of course, the front lines of medicine aren’t only where kids are getting sutured or where triage teams stop the bleeding; they run through the nurse’s station, through the community clinic, checking blood pressure for the thirty-fifth time, talking about disease with the day’s last patient. The front lines run all the way through to an exam table where we try to have a conversation about our future in the span of fifteen minutes. The scenes aren’t as dramatic, but the stakes are still high, where small choices have real consequences.
Knowing this, it’s easier to empathize with the doctor on the other side of the laptop, or with the nurses darting past the door. If the pandemic taught us anything, it’s that physicians and patients have a symbiotic relationship, and that any substantial reform to health care will be rooted in what doctors and patients find in common.